Surrogacy is far more than a medical process — it is a collaboration built on trust, compassion, and shared hope. As the Operations Head of a surrogacy agency, I stand at the intersection of medicine, logistics, law, and human emotion. My responsibility is to ensure that every part of this journey is safe, transparent, and deeply respectful of the people who make it possible.
Every surrogacy story begins with a dream, but it succeeds because of structure. Behind every ultrasound image, every legal document, and every joyful birth, there is a carefully coordinated system designed to protect the surrogate, nurture the baby, and keep intended parents close to the experience, even when they are thousands of kilometers away.
Our entire operational model rests on three principles:
- Safety – We protect the health of the surrogate and support the healthy development of the baby through structured medical monitoring, certified clinics, and evidence-based protocols.
- Transparency – Intended parents receive timely, clear updates at every stage. They know what is happening, why it is happening, and what comes next.
- Support – Both surrogates and intended parents deserve emotional and practical care. No one should ever feel alone in this journey. These principles guide every decision we make — from the very first consultation.
Surrogate mothers are the foundation of surrogacy.
They give their time, their energy, and their compassion to help another family grow. Our responsibility is to ensure they feel: Safe, Supported, Respected, emotionally understood, Protected legally and medically. Caring for a surrogate starts by building a relationship with them. Every question they ask reveals hopes and a sense of responsibility. Surrogates want reassurance that their well-being is a true priority, that their family will not be burdened, and that the birth will be handled with dignity and care. We honor that trust every single day.
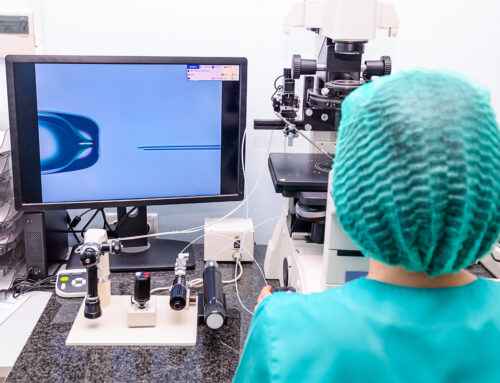
Antenatal Medical monitoring is an act of care.
Pregnancy care in the surrogacy journey begins with the earliest confirmations of pregnancy — moments filled with both excitement and tenderness. During the first trimester, surrogacy pregnancies receive a little extra attention. This is completely normal and is done to make sure the pregnancy is developing safely and that the surrogate feels well supported. These early weeks are delicate, and the additional checks help everyone feel confident and reassured.
- This stage includes β‑hCG testing,
- Early ultrasounds to confirm the heartbeat and healthy growth,
- Hormone checks to support a smooth pregnancy, and updated blood tests to ensure a safe environment for the baby.
- Around week 10, the surrogate may also have a genetic screening, such as NIPT (Non-invasive prenatal screening test), for early insight into the baby’s health if the intended parents wish for it. Generally, transferring PGT-A tested embryos significantly decreased the need for NIPT testing.
We share these first milestones with intended parents through structured updates and early ultrasound images, sometimes even organizing their attendance at ultrasound check-ups via video calls. Even after, they can feel the joy of seeing the first sign of new life — a moment that often becomes one of the most cherished memories of the entire journey.

Second Trimester management
As the pregnancy settles into a steady rhythm, the second trimester brings clarity, development, and beautiful details. Monitoring includes:
- Baby ultrasound scans and growth assessments (18–22 weeks)
- Maternal health evaluations and screenings for anemia.
Our team communicates every result with care and clarity. We make sure the surrogate feels supported, and the intended parents feel included and emotionally connected to their growing baby. This is often the stage where the journey feels real. Starting from week 12, we encourage communication between intended parents and surrogates, organizing video calls and ensuring there is a connection so IPs can be present and be involved at every stage of pregnancy.
Overcramming Challenges:
Despite excellent medical care, pregnancy can bring unexpected challenges, too. Depending on the situation, the medical team may recommend: Additional ultrasounds, more frequent monitoring, Medication adjustments, hospitalization of the surrogate, or specialist consultations. We coordinate every step, support the surrogate emotionally and practically, and keep intended parents updated with steady, clear communication. No matter when a complication appears, we aim to act quickly and compassionately, ensuring IPs give all needed info for decisions and even for arrival if needed. Premature delivery is sometimes expected, and the presence of intended parents at this stage is most important.
Preparation for Delivery
As the due date approaches, monitoring becomes more frequent and more focused. This stage includes:
- Growth scans every 3–4 weeks
- Blood pressure and urine checks,
- Fetal movement tracking and delivery planning with the chosen hospital.
It is always recommended that intended parents arrive in the destination country and meet the surrogate in person, starting from week 36. This time allows not only bond establishment but also to finalize needed legal paperwork, and gives Intended parents the possibility to attend several consultations before delivery. The plan is set, and attend to it if the medical team confirms and the surrogate feels comfortable. Before Travel, we are sharing a short guide for delivery preparation to IPs so they can have all the needed info upfront and be better prepared for a life changing moment in their lives.
We manage every detail — logistics, documentation, communication — so intended parents feel prepared and supported as the birth window draws near. This is a time filled with anticipation and emotion.
As Operations Head, I have learned that the true meaning of this work lies not in the systems we build, but in the lives we touch and every new life we create together with our medical team, and surrogates is a miracle, every smile on the intended parent’s face is precious. It means we did it.
Ketevan Tabutsadze, MD
Operations Head





Leave A Comment